We spent 25 days in Colchester NICU. She was stable and purely waiting for a bed at Great Ormand Street for the majority of her stay. She needed to be at GOSH for them to do a more detailed sleep study than Colchester could perform and for them to look at a more permanent nasal airway PLUS give us the training to manage said airway.
There were 2 occasions in those 25 days where a bed was suppose to be available but one time another baby needed it more than Rosie so she was back at waiting and the other time the baby who was due to be discharged relapsed and couldn't be moved anymore so Rosie continued to wait.
These 25 days were the longest in my life. It was awful not knowing how many more days or weeks we would be waiting. I was desperate to have her home and it was exhausting going to the nicu everyday for hours while I was still recovering my CS. The seats aren't comfy, the rooms are sweltering and there is buzzing and beeps going off all around you as babies have drops in their stats. It's not a nice place to be and my heart goes out to the parents who have this be their life for months.
Most of the babies in the NICU were preemies - it seems quite uncommon to have a full term baby in there. This made it extra hard as she was having period of becoming more and more alert but she was stuck in her crib - unable to be taken out for tummy time and be played with much due to wires and needing to be hooked up to monitors. Other babies who were premature mostly slept - so I started getting very upset about her missing out on social interaction. I was so desperate for her to come home.
During our wait for a bed at GOSH there was a time were Colchester NICU were thinking of discharging us with their temporary nasal airway and allow us to wait for GOSH as an outpatients, but suddenly that changed. It got all very confusing as so many professionals had different opinions and they were trying to communicate between Broomfield cleft team, Colchester hospital and GOSH.
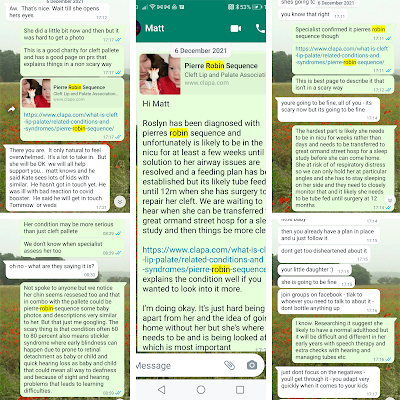
We made the best of it and tried to take photo's and videos each day to send to family. Her grandparents especially found it hard not being able to meet her and spent the first few weeks of her life getting to know her via photos. Unfortunately, due to covid only parents were allowed in the NICU - so no one other than us got to meet her.
First few weeks in the nicu:
First time in an open crib as oppose to an incubator at 2 days old as she was regulating her own temperature very well. Unfortunately, it didn't last long as she caught a cronobacter infection a few days after and was put back in an incubator to prevent spread as a cautionary measure. But I still remember feeling so proud seeing her in a "big girl crib"
NICU stay continued:
Rosie's first post from her cousins. They were excited to give her a birthday card for her BIRTH day!

Rosie passing her car seat stress test at 19 days old!

Christmas in the NICU obviously wasn't ideal and not the way we had thought we would spend the day as a new family of three.
Waking up it didn't feel like Christmas at all. But going in to the NICU that morning. we were greeted by gift bags on the incubator... Santa had been. What a lovely surprise! It made things feel slightly more Christmassy and it was beautiful to open presents with Rosie on her first Christmas. There were lovely gifts like rattles, children's books and gift cards in there and we had a great time going through everything. It felt like we were children ourselves as we opened things with Rosie. The gifts where donated by amazing charities such as wish upon a fairy (a charity that raises money for Colchester NICU)
The staff all dressed up and there were pretty decorations around us. It was the best that they could have made the day an I actually found myself really enjoying Rosie's first Christmas. Even Santa came to see us!
I'm so thankful to the charities and NICU staff for doing all they could to make the day special.